How Much Vitamin D Supplementation Do I Need?
How Much Vitamin D Supplementation Do I Need?
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
Supplementation with krill oil, fish oil or cod liver oil has been a traditional recommendation-but maybe not the best recommendation with new scientific studies. Any supplements with levels of over 3000 I.U. of retinol should be avoided. Magnesium, Vitamin K, boron and zinc are recognized co-factors for synthesizing Vitamin D. Recommendations are running in a range from 2000 with a few suggestions for 10,000 once a week, while the RDA is still at 400 I.U. I believe you must supplement, but be careful not to overdose on these supplements. Have your Vitamin D levels checked if you want to take the higher end doses. Most alternative practitioners are suggesting 2000 – 5000 I.U. with an occasional dose of 10,000 every 3 weeks. Others suggest a large dose when fighting a cold.
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.
Do Not Depend on Food Sources for Vitamin D
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
Food sources of Vitamin D are very inadequate. A list is included for comparison. Remember, the suggested daily intake is now in the 2000-5000 I.U. range daily. Fifteen minutes in the sun can provide a 10,000 I.U. boost when the proper guidelines are followed. Be careful of products that are fortified. They give a false sense of security that you have gotten your Vitamin D that day because you ate a particular food. Most of the fortified foods are of course given a boost of Vitamin D that is synthetic. Synthetic is not the same as a natural source.
Data in the following list is gathered from U.S. Department of Agriculture, Agricultural Research Service.
USDA Nutrient Database for Standard Reference, Release 22, 2009.
Selected Food Sources of Vitamin D |
||
| Food | IUs per serving* | Percent DV** |
| Salmon (sockeye), cooked, 3 ounces | 794 | 199 |
| Mackerel, cooked, 3 ounces | 388 | 97 |
| Tuna fish, canned in water, drained, 3 ounces | 154 | 39 |
| Milk, nonfat, reduced fat, and whole, vitamin D-fortified, 1 cup | 115-124 | 29-31 |
| Orange juice fortified with vitamin D, 1 cup (check product labels, as amount of added vitamin D varies) | 100 | 25 |
| Yogurt, fortified with 20% of the DV for vitamin D, 6 ounces (more heavily fortified yogurts provide more of the DV) | 80 | 20 |
| Sardines, canned in oil, drained, 2 sardines | 46 | 12 |
| Liver, beef, cooked, 3.5 ounces | 46 | 12 |
| Ready-to-eat cereal, fortified with 10% of the DV for vitamin D, 0.75-1 cup (more heavily fortified cereals might provide more of the DV) | 40 | 10 |
| Egg, 1 whole (vitamin D is found in yolk) | 25 | 6 |
| Cheese, Swiss, 1 ounce | 6 | 2 |
* IUs = International Units.
** DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet. The DV for vitamin D is currently set at 400 IU for adults and children age 4 and older. Food labels, however, are not required to list vitamin D content unless a food has been fortified with this nutrient. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
Getting The Most From Your Vitamin D Supplement
Why You Should Avoid Cod Liver Oil and Vitamin A and D combinations
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
The British Medical Journal published a paper that confirmed low vitamin D levels are a risk factor for developing colon cancer in the future. However, the most remarkable part of the paper is that the 46 scientists minimized the true importance of their own research. They found that vitamin A, even in relatively low amounts, appears to thwart vitamin D’s association with reduced rates of colon cancer.
This was a prospective nested case-controlled study, which means it used subject’s vitamin D blood samples obtained and frozen in the past and then reviewed their medical records into the future to see who gets colon cancer, comparing the study subjects to similar members of the group that did not get the illness. Dr. Mazda Jenab and his 45 colleagues from the International Agency for Research on Cancer confirmed that low vitamin D levels are a risk for colon cancer in a dose response manner; those with the highest levels were about twice as likely to develop colon cancer compared to those with the lowest levels.
The largest study to date on pancreatic cancer showed vitamin A blocks vitamin D’s effect and explains some of the anomalies in other papers on vitamin D and cancer. The first paper by Dr.Rachael Stolzenberg-Solomon of the NIH showed high vitamin D levels tripled the subsequent risk of pancreatic cancer. The research was done in Finland with high cod liver oil intakes. A second paper showed no effect. The study was done in the US with no appreciable cod liver oil intake.[1]
Ten similar studies have been conducted on vitamin D blood levels and the risk of subsequent prostate cancer. Dr. Lu Yin of the German Cancer Research Center reviewed them in detail. Two studies from Nordic countries showed increased rates of prostate cancer with high Vitamin D levels.[2]
Dr. Cannell also states, “So it is not just autistic children that are being harmed by vitamin A. Avoid cod liver oil like the poison it is and check your multivitamins. Life Extension Foundation just reformulated their multivitamin to contain only 500 IU of preformed retinol. And, I am happy to report that Purity Products, which markets my vitamin D, has no preformed retinol at all in any of their multivitamins, only beta-carotene. Purity has also stopped selling cod liver oil. Now, if only Carlson, Solgar, Nature’s Way, and other companies would stop selling cod liver oil and stop selling their concentrated vitamin A supplements to a country whose problem is widespread sub-clinical vitamin A toxicity, I’d be a happier agitator.” [3]
Where Can I Get My Vitamin D?
Vitamin D3 supplements come in several forms:
- oil (cod liver oil-based) – fat-soluble vitamin D, includes liquid drops or gel caps
- liquid drops (lanolin-based) –fat-soluble vitamin D
- dry powder (lanolin-based) – water-soluble vitamin D, includes capsules or tablets.
- As far as we know, both water-soluble and fat-soluble vitamin D are equally absorbed and metabolized by the body, and are thus equally effective.
- Breast cancer affects about 210,000 females each year compared to 2,000 men. Approximately 20% of those diagnosed with breast cancer die from the disease. One of the best gifts you can give anyone with cancer, especially breast cancer is a supply of the correct kind of Vitamin D3.[1] Stolzenberg-Solomon RZ, et al. A prospective nested case-control study of vitamin D status and pancreatic cancer risk in male smokers. 15;69(4):1439–47.
[2] Yin L, Raum E, Haug U, Arndt V, Brenner H. Meta-analysis of longitudinal studies: Serum vitamin D and prostate cancer risk.
[3] http://www.vitamindcouncil.org/news-archive/2010/vitamin-d-vitamin-a-and-cancer/
Vitamin D Recommendations Change Often
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
It’s hard to keep up with the changes in recommendations for Vit. D. A gradual increase in Vit. D is step towards better health in many areas. But as always moderation is needed. It seems to me that more studies on the correct amount needed to protect us should be completed. Several websites include information about huge amounts of Vitamin D being safe. I do not feel this is correct: everything should be in moderation. Our liver will be called on to detoxify this extra vitamin D and it does not matter if it is from a natural or synthetic source. It can only detoxify small to moderate amounts, not mega doses. We need to be getting moderate amounts of sunlight daily and moderate amounts of supplements. Our body will use what it needs.
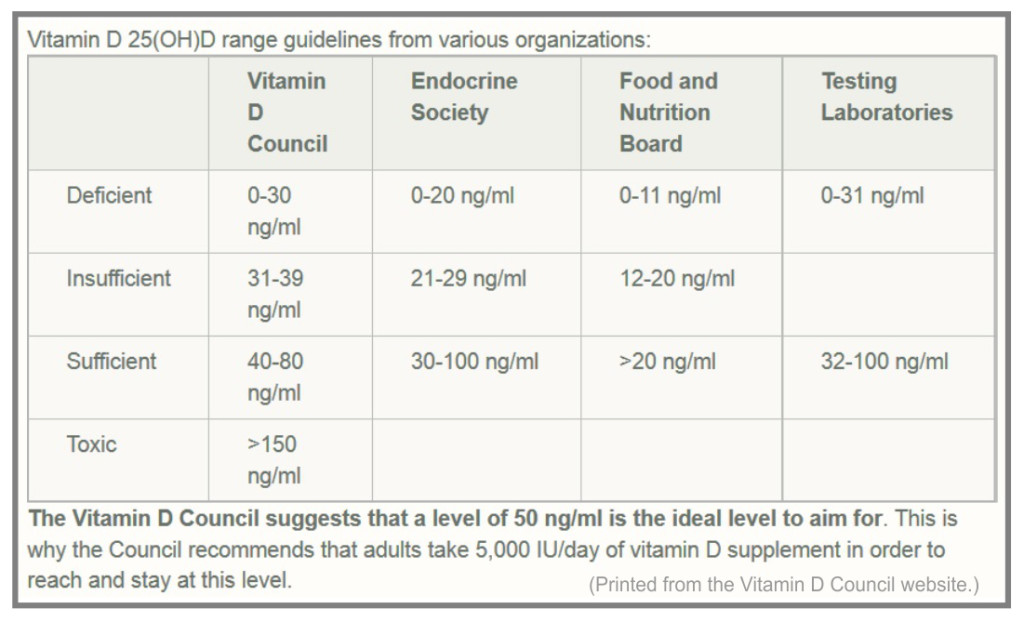
Dr. John Cannel, founder of the Vitamin D council, stated,” My advice, especially for pregnant women: continue taking 5,000 IU/day until your 25(OH)D is between 50–80 ng/mL (the vitamin D blood levels obtained by humans who live and work in the sun and the mid-point of the current reference ranges at all American laboratories).
How do I Test My Vitamin D Level?
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
A visit to www.vitamindcouncil.org is a must at this point. They have partnered with Heartland Assays for an In-home vitamin D test. This is an inexpensive in-home Vitamin D test, the least expensive one in the United States!
What to expect
Heartland Assays’ Vitamin D Kit is suitable for use with adults and children. When using the this test kit you will find the procedure to be both simple and straightforward:
- Purchase the test kit from the Vitamin D Council website. The cost is $50 for 1 test kit and $180 f0r a 4 pack, with additional shipping charges.
- Once the test kit is received, and when ready, follow the instructions in the kit, and/or watch this video (scroll down). The test is simply a finger prick with a lancet, with the samples (blood drops) to be placed on the included blotter paper.
- No additional fee is required for domestic orders — the test results will ne posted on your personal account on the Vitamin D Council website.
For optimum health, vitamin D blood levels should be around 50-80 ng/mL (125-200 nmol/L).
Reference ranges represent the range of values that the majority of the population will fall between and are not indicative of values which would be considered optimal. Studies indicate that for proper health, serum vitamin D levels should be a minimum of 50 ng/mL (125 nmol/L), with optimal levels falling between 50-80 ng/mL (125-200 nmol/L). These values apply to both children and adults.
Protection Roles of Vitamin D
Over 40 ways the Vitamin D contributes to good health!
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
(Note: The amount of Vitamin D produced naturally in your body varies in different geographical locations and in different seasons. If you have adequate sun exposure in the summer months, do not take supplements. Rotate the supplements seasonally.)
In lab and animal tests, vitamin D stifles abnormal cell growth, curbs formation of blood vessels that feed tumors and has many other anti-cancer effects. It may increase the self-destruction of mutated cells, reduce the reproduction of cancer cells and actually cause them to become differentiated—which is a good thing.
Vitamin D helps your immune system T-cells to change shape and migrate to the top layer of your skin to destroy damaged and infected cells. This may be why Vitamin D has such a protective effect against skin cancer.
Enough sun exposure also increases blood levels of white blood cells that destroy the cell walls of viruses and bacteria. A newer remedy for coughs and colds is simply extra Vitamin D supplements taken at 5000 I.U. for three days at the onset of a cold.
Vitamin D is not actually a vitamin—it’s produced from cholesterol and labeled a pro hormone. Most cells in your body have a Vitamin D receptor indicating the enormous problems that could arise when your intake of this vitamin has been drastically reduced with the “slip, slap and slop” mentality of sunscreen manufacturers.
It’s proven it countless studies that Vitamin D is best when naturally absorbed by the skin, where it is stored in a fat layer right under the skin. Our body uses this storehouse in declining sunny months to protect us from a variety of health issues.
Vitamin D deficiency is linked to:
16 types of internal cancers
Autism
Colds and flu
Depression
Diabetes
Heart disease
Hypertension
Low energy and fatigue
Lowered immunity
Mood Swings
Multiple sclerosis
Muscle pain
Psoriasis
Respiratory ailments
Rickets
Schizophrenia
Sleep irregularities
Tuberculosis
Myopathy
Weak bones/fractures
rickets
osteomalacia
osteoporosis
Women with renal problems or intestinal concerns (such as IBS or Crohn’s disease) may be vitamin D deficient because they can neither absorb nor adequately convert the nutrient.
Avoiding Sunlight May Be Killing You
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
We need to carefully assess our skin cancer risks. From what information I could find, we have been scared out of the sun needlessly. It seems that non-melanoma skin cancer (the reason we stay out of the sun and cover ourselves with chemicals) causes about 1,200 deaths– only two-tenths of 1 percent of all the cancer deaths in America each year. It’s also interesting that mortality rates for melanoma rose steeply after sunscreens came into common use, not before.
But it is estimated that additional exposure to vitamin D would save almost 350,000 cases of breast cancer worldwide.[1] Approximately 1,150,000 cases and 410,000 deaths from breast cancer occur annually worldwide, including 215,000 new cases and 41,000 deaths in the United States according to the May-June issue of the Breast Journal. Some estimates are that half of these cases could be prevented. It is estimated that 50,000-63,000 individuals in the United States, and 19,000-25,000 in Great Britain, die prematurely from cancer annually due to insufficient vitamin D.[2]
On the flip side, ““While ultraviolet B radiation from the sun is the primary source of vitamin D in our body, unprotected sun exposure is not a recommended way to reduce a person’s risk of developing breast cancer,” said David J. Leffell, M.D., Yale Cancer Center member and Professor and Section Chief of Dermatologic Surgery at Yale School of Medicine.
Accepted ways to decrease a woman’s risk of breast cancer include avoidance of weight gain, moderation in alcohol consumption if any, regular physical activity, and a healthy and balanced diet, say the Yale experts.”[3] I’m having a hard time even printing this statement—it sure hasn’t improved our statistics so far. We have to go way beyond those simple statements to decrease our breast cancer risks. But I am trying to show there are always two sides to consider.
We have traded sunscreen “protection” for a huge increase in other cancers, especially breast, colon, lung and prostate. Honestly, how could we have survived as a race for thousands of years without all the clothing and sunscreen that we have today? That’s like saying that God doesn’t know what he is doing. This really doesn’t make sense to me! So I have been thrilled with all the new research about the benefits of the sun and Vitamin D.
As always….money and greed have played a big role in this scare.
_______________________________________________________________________________________________________________
[1] Mercola, Joseph. Over A Million People Die EVERY Year From Lack of Sun Exposure: A Special Report http://www.mercola.com/Downloads/bonus/benefits-of-sun-exposure/report.htm
[2] Photobiology 81: 1276-86, 2005
[3] Yale University (2008, May 18). Increasing Sun Exposure Is Not The Way To Decrease Breast Cancer Risk, Despite New Data, Warn Cancer Experts. ScienceDaily. Retrieved December 1, 2008, from http://www.sciencedaily.com /releases/2008/05/080515102017.htm
Moderate Sun Exposure Provides Protection
from Teaching Series by Linda Bamber, founder of Breast Research Awareness and Support
(Note: The amount of Vitamin D produced naturally in your body varies in different geographical locations and in different seasons. If you have adequate sun exposure in the summer months, do not take supplements. Rotate the supplements seasonally.)
Ladies, it’s not that hard to get out in the sun. We need to gradually expose ourselves 10-15 minutes a day over 40% of our body to give us enough Vitamin D for breast cancer protection. Dark pigmented skin needs 3-6 times longer exposure for the same beneficial protection.
New updates are indicating that once we have been in the sun and are intentionally trying to build up our Vitamin D levels, that we need to refrain from washing all this goodness off for at least 24-48 hours. That means a shower without soap is needed to allow our skin to manufacture the Vitamin D. If we use soap it negates the sunlight we have absorbed.
It couldn’t be easier said. We just need to clear our thoughts and remember when sunlight was considered good for us. It still is, and it always has been.
I’m not sure when Americans developed a phobia against the sun. “It will cause skin cancer. I burn easy…” I actually do remember tanning a lot when I was in my teens in the late 1960’s. My sister and I drove a tractor on the family farm and we always had to flip a coin to see who got the tractor without the umbrella so we could tan. Luckily-we didn’t seem to burn after hours in the sun –maybe all the dirt and dust protected us. Probably it was the fresh garden produce (full of antioxidants) and the correct omega 3’s from dairy sources that are both known to protect us from skin cancer. But when my children were born over a decade later…you were considered a terrible mother if your children weren’t slathered with sunscreen.
The variety of sun blockers available to “protect our skin” from damaging UV light is mind-boggling. Most of them have now been proven to add to the problem: flooding our body with damaging, cancer-causing chemicals instead. Those chemicals, layered on our skin, are more damaging to our system than chemicals or pesticides that we ingest daily. Anything placed on our skin will go directly into our bloodstream, whereas, food we eat will be metabolized by the liver. Unfortunately many of us do not have very strong functioning livers.
Make time in your day for the sun. You’ll get some color and people will rave about your youthful appearance from just a little sun. If you live in an area with little sunshine- you have several options.
Do not expect Vitamin D milk to be of any help for your body. It is a synthetic form of D2 or ergocalciferol and therefore not the right kind of vitamin D.
[1] Bérubé S, Diorio C, Verhoek-Oftedahl W, Brisson J, Vitamin D, calcium, and mammographic breast densities. Cancer Epidemiol Biomarkers Prev. 2004 Sep;13(9):1466-72.
[1] Mercola, Joseph. Over A Million People Die EVERY Year From Lack of Sun Exposure. A special report by Mercola. <Mercola.com>.
Vitamin D Protects Us from Breast Cancer
from Teaching Series by Linda Bamber, 2007, updated June 2011
“Higher serum levels of vitamin D are associated with reduced incidence rates of breast cancer worldwide,” said Cedric F. Garland, Dr. P.H., professor of Family and Preventive Medicine in the UCSD School of Medicine, and member of the Moores UCSD Cancer Center.[1] They used GLOBOCAM, a database of cancer incidence, mortality and prevalence for 175 countries to chart cancer rates and latitudes. A clear association between deficiency in exposure to sunlight, specifically ultraviolet B (UVB), and breast cancer was plotted.
“This is like the Holy Grail of cancer medicine; vitamin D produced a drop in cancer rates greater than that for quitting smoking, or indeed any other countermeasure in existence.”
~ Dennis Mangan, clinical laboratory scientist[2]
Studies Verify Protection
A Canadian study followed 512 women after diagnosis of breast cancer. Those who were deficient were nearly twice as likely to have their cancer recur or spread over the next 10 years, and 73 percent more likely to die of the disease. “These are pretty big differences,” said study leader Dr. Pamela Goodwin of Mount Sinai Hospital in Toronto. “It’s the first time that vitamin D has been linked to breast cancer progression.”[3]
The Canadian study was paid for by the Breast Cancer Research Foundation in New York, established by cosmetics magnate Evelyn Lauder. “It’s a very provocative paper. It’s confirmatory of a tremendous amount of evidence that vitamin D is an important component of health,” said Dr. Larry Norton, chief of breast cancer programs at Memorial Sloan-Kettering Cancer Center in New York and a medical adviser to the foundation.
Other studies conclude that women who had more exposure to sun during puberty, or who have high intakes of the vitamin as adults, are less likely to develop breast cancer. [4]
A study in Norway including 115,096 cases of breast-, colon- or prostate cancer, studied geographical locations and seasonal variations at diagnosis. Among these, 45,667 deaths due to the cancer were registered and a correlation with seasonal variations noted. “The results suggest that a high level of vitamin D(3) at the time of diagnosis, and thus, during cancer treatment, may improve prognosis of the three cancer types studied.” [5]
Vitamin D and calcium are being evaluated as potential breast cancer prevention agents. Studies have shown Vit. D and calcium can decrease mammographic breast densities, one of the strongest breast cancer risk factors.[6] Another study revealed that Vitamin D and calcium did not protect us from breast cancer—but a closer look revealed that they used a daily intake of 400 I.U. when all the newer studies are clearly showing that we need 2000-5000 I.U. daily. Another study from Indonesia found that treating tuberculosis patients with 10,000 I.U. of Vitamin D daily led to a cure rate of 100%. [7]
The Vitamin D Council provides a great overview of studies done connecting breast cancer and low Vitamin D levels. Dr. John Cannell, the Director has been the leader in Vitamin D education for years. Access their website at http://www.vitamindcouncil.org/cancerBreast.shtml for more information and studies.
____________________________________________________________________________________________
[1]University of California – San Diego. “Link Between Vitamin D Status And Breast Cancer Illuminated.” ScienceDaily 16 May 2008. 28 November 2008 <http://www.sciencedaily.com /releases/2008/05/080515174000.htm>.
[2] http://www.vitamindcouncil.org/health-conditions/cancer, accessed June 2011.
[3] http://www.cnn.com/2008/HEALTH/conditions/05/16/vitamind.breast.cancer.ap/index.html
[4] Vitamin D linked to lower breast cancer risk, Stephen Daniells, 04-Apr-2006, http://www.nutraingredients-usa.com
[5] Robsahm TE, Tretli S, Dahlback A, Moan J, Vitamin D3 from sunlight may improve the prognosis of breast-, colon- and prostate cancer. Cancer Causes Control. 2004 Mar;15(2):149-58
[6] Bérubé S, Diorio C, Verhoek-Oftedahl W, Brisson J, Vitamin D, calcium, and mammographic breast densities. Cancer Epidemiol Biomarkers Prev. 2004 Sep;13(9):1466-72.
[7] Mercola, Joseph. Over A Million People Die EVERY Year From Lack of Sun Exposure. A special report by Mercola. <Mercola.com>.
What is Breast Cancer?
An informative article cited in Linda Bamber’s research on Vitamin D
from the Vitamin D Council, last updated October 15, 2015
Tumors are made when there is a buildup of unneeded, old or damaged cells that form a mass. Breast cancer is a malignant tumor, which is a group of cancerous cells that can grow and spread to surrounding tissues. If the cancer spreads away from the breast cells to other areas of the body, this is called metastasizing.
Breast tumors can either be benign or malignant. Benign tumors are usually not harmful, whereas malignant tumors are and can spread to other parts of the body. When breast cancer cells spread, they usually first spread to the lymph nodes, which are located at the underarms and above the collarbone. Read More >>